Researchers from HMRI’s Drug Repurposing Research Program are currently waging a two-pronged attack on ovarian cancer.
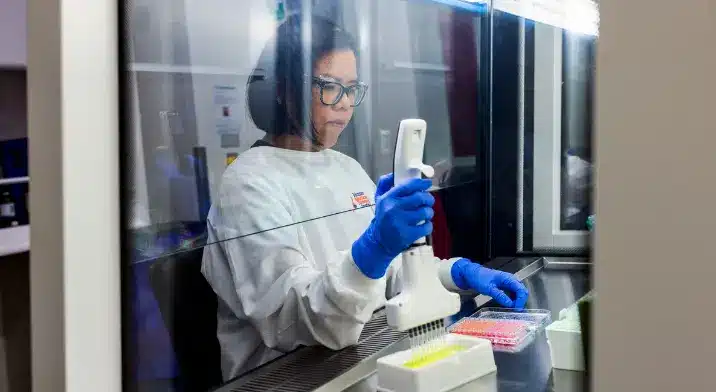
Dr Michelle Wong-Brown says that their research started out trying to find new drugs for treatment-resistant ovarian cancer.
A lot of ovarian cancers are detected late and subsequently recur because they have metastasised, meaning that these patients get bombarded with chemo to try and slow the progress of the disease.
The drugs that are currently being used to treat this cancer are decades old and, while they do work for some, many women’s cancers become treatment-resistant over time.
Dr Wong-Brown and her team, including PhD candidate, Bayley Matthews, who was the recipient of the Jill Emberson Scholarship for Ovarian Cancer research, have found a drug that seems to work – they just don’t why.
“Bayley was meant to spend a year trying to figure out why this drug works on treatment-resistant ovarian cancer. It’s been three years and we’re still trying to understand it,” says Dr Wong-Brown.
The drug, an off-patent HIV drug, is ready to go into a Phase1B clinical trial that has been endorsed by clinicians and consumer advocates.
The only thing stopping the trial is a lack of funds.
Dr Wong-Brown says that the drug is cheap but the process of running a multi-site clinical trial is expensive.
“We need at least $100,000 to get this off the ground. Once we start the trial, we need to recruit around 40 people with treatment-resistant ovarian cancer to trial the drug for safety and efficacy,” says Dr Wong-Brown.
In addition to finding a promising new drug for treating ovarian cancer, the team are also working on an early-detection blood test.
“It’s called a liquid biopsy.
“We’re trying to see if there are any markers that show up in the early stages of ovarian cancer,” says Dr Wong-Brown.
PhD candidate Sara Atiq is working on this and is combining lots of datasets from around the world to build the necessary sample size.
“If we find something that looks promising, we will then look at developing a sequencing test,” says Dr Wong-Brown.
This work will be conducted in partnership with the cancer biobank and will involve recruiting patients that are going for surgery for suspected ovarian cancer.
The sequencing test would be run on blood samples from the patient before their pathology diagnosis comes back from the lab. Then, the pathology diagnosis would be cross-matched with the results of the sequencing test to see if the test is accurately diagnosing the presence of ovarian cancer.
Four years in the making
Dr Wong-Brown says it’s taken them four years to get to this point.
“From testing drugs on ovarian cancer cells, to better understanding the role of PARP- a protein (enzyme) found in our cells that helps damaged cells to repair themselves – and gene mutations in treatment-resistant ovarian cancer, it’s taken four years, $40,000 in pilot funding from HMRI and and the Medical Research Future Fund (MRFF).
HMRI would like to acknowledge the Traditional Custodians of the land on which we work and live, the Awabakal and Worimi peoples, and pay our respects to Elders past and present. We recognise and respect their cultural heritage and beliefs and their continued connection to their land.
Hunter Medical Research Institute
We’re taking healthy further.
Locked Bag 1000
New Lambton
NSW, Australia, 2305


This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Copyright © 2024 Hunter Medical Research Institute | ABN: 27 081 436 919
Site by Marlin Communications
