The largest ever genomic study of pneumonia has identified the genetic risk signals of the disease, paving the way for potential new treatments and the use of precision medicine.
The largest ever genomic study of pneumonia has identified the genetic risk signals of the disease, paving the way for potential new treatments and the use of precision medicine.
Precision medicine is a treatment approach that takes into account individual variability in genes, environment, and lifestyle for each person, allowing doctors and researchers to predict more accurately which treatment and prevention strategies for a particular disease will work in which groups of people.
The development of a quick, straightforward genetic test of a patient with pneumonia could determine the best drug therapy for them based on their pneumonia susceptibility.
In a parallel and unexpected finding the University of Newcastle study, published in Nature Communications, also discovered a genetic correlation between risk of pneumonia and risk of psychiatric disease, such as schizophrenia, bipolar disorder and major depression.
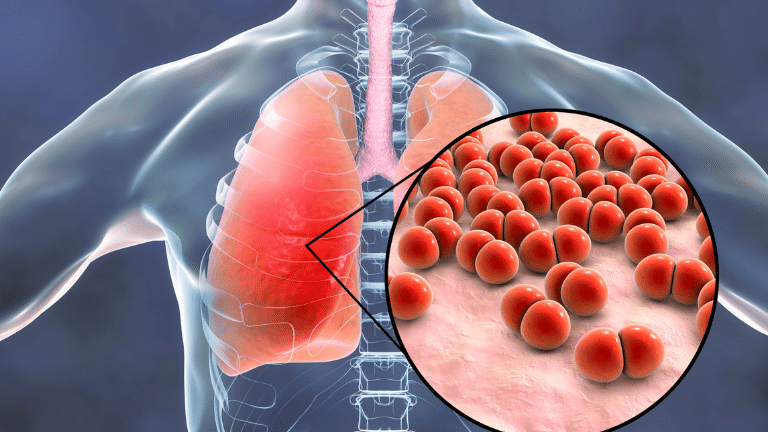
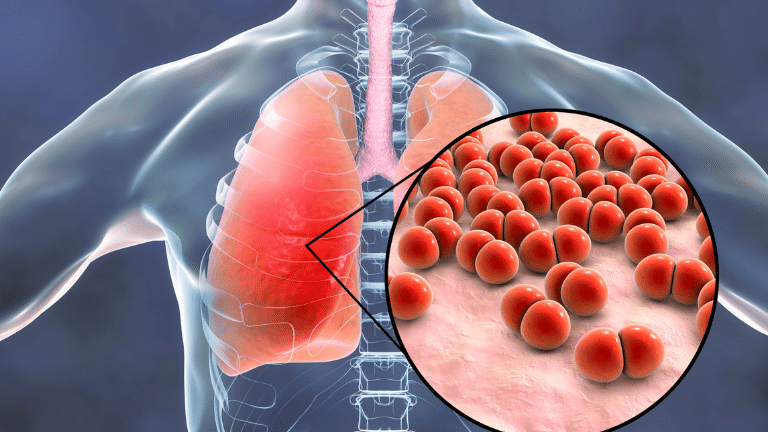
Pneumonia is considered one of the worst outcomes for any kind of respiratory condition or infection. Characterised as an acute infection of the lung, with fluid or pus-filled alveoli causing an extreme restriction of oxygen intake, it remains one of the leading causes of death worldwide.
A number of mechanisms cause pneumonia, however, bacterial or viral infection are the most common. Bacterial-induced pneumonia is treated with antibiotics, yet yearly mortality rates worldwide remain high, even in developed countries where access to antibiotics and routine hospital care are usually available.
Principal Investigator, University of Newcastle Professor Murray Cairns, from the HMRI Precision Medicine Research Program, said current treatments were not effective for all pneumonia patients or suitable as a ‘one drug suits all’ medical response.
“Every year thousands of people die with influenza, yet it is pneumonia that kills them. And, many patients hospitalised for COVID-19 throughout the pandemic have been treated for pneumonia as well.
“It is a terrible condition where people often need hospitalisation and intensive care including intubation and mechanically assisted ventilation. There is also a further risk of multiple-organ failure and death,” he said.
Precision medicine
Professor Cairns said pneumonia was a complex disorder and people inherited different patterns of risk for the condition.
The genome-wide association study, which interrogated data from the 23andMe study and FinnGen consortium, identified four new genomic regions with genes associated with the risk for pneumonia.
The team then focused on identifying drug targets which would most likely be helpful in treating the condition.
“We were able to not only recognise drugs that could help with this disorder, but also find a way to tailor those treatments specifically to an individual’s specific risk or susceptibility for the disorder.
“This is what we commonly call precision medicine because we can tailor the treatment to suit the person’s underlying biology.
“Precision medicine is far more effective than having just one drug for pneumonia as the response varies tremendously from one individual to another due to their underlying risk factors – both environmental and genetic.”
Link to psychiatric disease
The study also found a compelling and unexpected genetic correlation between risk of pneumonia and risk of psychiatric illness.
“Following the genetic analysis where we looked at the relationship between thousands of variants across the genome and the risk for pneumonia, we then compared that risk with all other diseases.
“One of the closest relationships to pneumonia we found were with psychiatric disorders such as post-traumatic stress disorders, major depression, attention deficit hyperactivity disorder, and schizophrenia.
“I think it’s surprising, but in some ways it’s not, as there are thought to be inflammatory risks for mental illness.
“It is a well-known risk factor for psychiatric illness so it’s potentially a risk shared between those disorders.”
‘The genetic architecture of pneumonia susceptibility implicates mucin biology and a relationship with psychiatric illness’ was published in Nature Communications. The lead author of the study is Dr William Reay.
HMRI would like to acknowledge the Traditional Custodians of the land on which we work and live, the Awabakal and Worimi peoples, and pay our respects to Elders past and present. We recognise and respect their cultural heritage and beliefs and their continued connection to their land.

Hunter Medical Research Institute
We’re taking healthy further.
Locked Bag 1000
New Lambton
NSW, Australia, 2305



This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Copyright © 2024 Hunter Medical Research Institute | ABN: 27 081 436 919
Site by Marlin Communications
