Breast cancer statistics in Australia: Breast cancer is the second most commonly diagnosed cancer in Australia and the most common among women, with a 24% increase in diagnoses over the past 10 years. However, the mortality rate has decreased by 40% due to better awareness, prevention, and treatment.
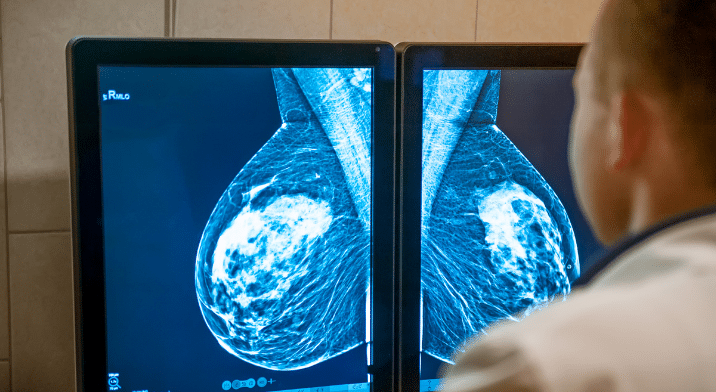
Mammography as a screening tool: Mammograms, recommended for women aged 50-74 every two years, are the primary method for early breast cancer detection. They work by compressing the breast tissue to detect abnormalities using low-dose X-rays.
New comfortable screening technique: Researchers are developing a new method using red and infrared light to image breast tissue, which could make breast cancer screening more comfortable and safer by avoiding radiation and breast compression.
Breast cancer is the second most commonly diagnosed cancer in Australia, and the most common cancer diagnosed in women. Over the past 10 years, diagnosis has increased by 24%, but the mortality rate decreased by 40% due to increased awareness, prevention, early-detection, and more effective treatments.
When it comes to early-detection, mammography is the recommended screening tool for breast cancer, with the current guidelines recommending women aged 50 – 74 years old have one every two years.
A mammogram is a low-dose x-ray of the breast which allows health professionals to identify any abnormalities or changes in the breast tissue over time. They work by compressing each breast, one-at-a-time between two x-ray plates, allowing the breast tissue to be spread out to give optimum visibility.
While mammograms don’t hurt, some people do experience some discomfort, and a team of University of Newcastle and HMRI researchers have been working on a new, comfortable way to screen for breast cancer.
Instead of using the usual ‘squishing’ of mammograms, cancer researchers Associate Professor John Holdsworth, Dr Renee Goreham and PhD candidate Catherine Merx, are looking at using red and infrared light to image the breast tissue.
Dr Goreham says, “Think of it like using a flashlight to see through your hand, but much more advanced. This technique could make breast cancer screening more comfortable, accessible and encourage more women to get checked.”

Catherine, who has been working on the project for the past year-and-a-half, has been testing the technique on gelatine with resin inserts.
“We’re managing to image to a few centimetres depth. In time, we’re hoping to be able to tell the difference between masses of different densities.” she says.
Unlike a mammogram that uses low levels of electromagnetic radiation, this technique measures the scattered photons from the red light to digitally reconstruct the mass that is obstructing the light waves.
Dr Goreham says, “It’s completely safe because there’s no radiation. There’s no squishing and it could be very portable. We also think it could be used outside of medicine to detect fruit flies in fruit or check the viability of eggs.”
So what are the next steps?
Dr Goreham says, “What Catherine has done so far is confirm that she can reconstruct scattered red light into an image that resembles what she had in the gelatin samples. The next step is to improve the resolution by improving the instrumental setup. For example, a better quality camera and confirming that images can be reproduced from materials that better mimic our body tissue – similar to that use for radiotherapy (phantom materials).”
HMRI would like to acknowledge the Traditional Custodians of the land on which we work and live, the Awabakal and Worimi peoples, and pay our respects to Elders past and present. We recognise and respect their cultural heritage and beliefs and their continued connection to their land.
Hunter Medical Research Institute
We’re taking healthy further.
Locked Bag 1000
New Lambton
NSW, Australia, 2305


This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Copyright © 2024 Hunter Medical Research Institute | ABN: 27 081 436 919
Site by Marlin Communications
