Professor Craig Pennell is the Chair in Obstetrics and Gynaecology and Professor of Maternal Fetal Medicine at the University of Newcastle, and a Senior Staff Specialist in Maternal Fetal Medicine at John Hunter Hospital. He is also the Co-Director of the Mothers and Babies Research Program at the Hunter Medical Research Institute.
In addition to his subspeciality training in maternal fetal medicine, he has a PhD in fetal physiology and completed postdoctoral training in molecular genetics in Toronto.
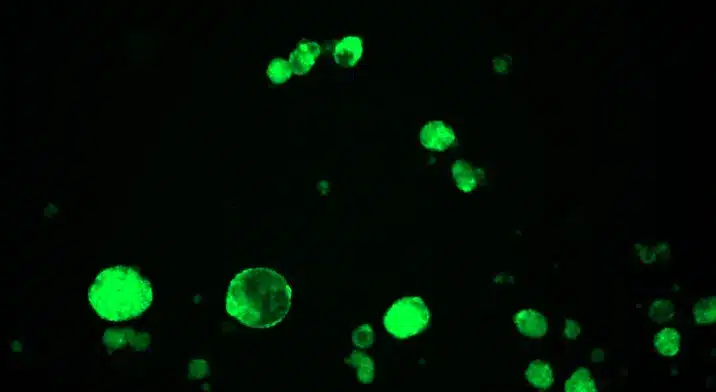
Professor Pennell’s research is best categorised as personalised medicine in perinatal health and the developmental origins of health and disease. His research is focused on the use of genetics and genomics to predict and prevent preterm birth and other pregnancy complications, as well as non-communicable diseases across the lifespan.
Professor Pennell has managed high-risk pregnancies as a subspecialist for over 20 years, and his clinical work focuses on the management of high-risk pregnancies, preterm birth prevention, stillbirth prevention and the early origins of health and disease.
In addition to research, teaching and clinical medicine, he is the Foundation Scientific Director of the Newcastle 1000 Family Study (NEW1000) and Chair of the National Scientific Advisory Group of Red Nose.
Over his research career, he has published more than 300 papers, been cited more than 22,000 times, and been awarded more than $33M in competitive research grants.