
Oh no! You were feeling a bit unwell and the test has come back positive for the dreaded COVID-19. What do you do now? We asked three of HMRI’s top researchers and teams for their tips on how to take care of yourself or your loved ones who have been diagnosed with the virus.

Oh no! You were feeling a bit unwell and the test has come back positive for the dreaded COVID-19. What do you do now? COVID-19 can be a serious illness and if you are experiencing serious symptoms, you should discuss it with your doctor or go to the hospital.
But for many people, especially those who are fully vaccinated, you will most likely be told to isolate, and self-manage at home.
So, what do you do when you are stuck at home in isolation and not feeling great?
We asked three of HMRI’s top researchers and teams for their tips on how to take care of yourself or your loved ones who have been diagnosed with the virus.
General tips
We know COVID-19 is highly contagious! Things that will help reduce your risk of getting it include:
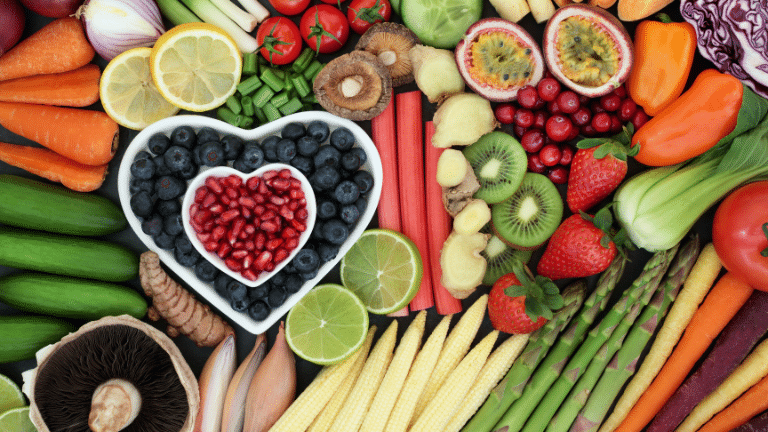
Give your body the right fuel to fight infection, with Laureate Professor Clare Collins
Since there is a lot of COVID-19 circulating in our community it’s a good idea to think ahead and make sure you have enough food in the house to survive a 7-day isolation while you recover.
If your goal is to avoid the supermarket, make sure you are well stocked with the staples.
Professor Collins and her team have put together some excellent resources on their website Nomoneynotime.com.au including:
“You can also tweak what you eat to help your immune system do its job in fighting infection. This means ensuring you regularly eat foods rich in the vitamins and minerals needed for your immune system to work efficiently,” Professor Collins said.
Check this table for the major nutrients needed by your immune system and the foods they are found in.
| Nutrient | Food Sources | Role in Immunity |
| Vitamin A | Oily fish, egg yolks, cheese, tofu, nuts, seeds, whole grains, and legumes |
Antibody production, maintenance of healthy lungs and gut. |
| Beta-carotene | Pumpkin, sweet potatoes, carrots, leafy green vegetables. |
Converted into Vitamin A by the body. |
| B Vitamins | ||
| B6 | Cereals, legumes, green leafy vegetables, fruit, nuts, fish, chicken, meat. |
Needed to produce antibodies and help reduce inflammation. |
| B9 (Folate) | Green leafy vegetables, legumes, nuts, seeds. Added to commercial bread-making flour. |
Promotes resistance to infection. |
| B12 (cyanocobalamin) | Eggs, meat, dairy, fortified soy milk (check nutrition information panel). |
Needed to make an immune response. |
| Vitamin C | Oranges, lemons, limes, berries, kiwifruit, broccoli, tomatoes, and capsicum. |
Needed for production of specialised cells (neutrophils, lymphocytes, phagocytes) that all help fight pathogens. |
| Vitamin E | Nuts, green leafy vegetables, vegetable oils. | Helps protect cells from oxidative stress. |
|
Vitamin D |
Eggs, fish, some milks, and margarines are fortified with added Vitamin D. People with Vitamin D deficiency may need supplements. |
Used by some immune cells to help destroy pathogens. |
| Minerals | ||
| Iron | Meat, chicken, fish, legumes, whole grains, iron-fortified breakfast cereals. |
Regulates pathways that help immune cells recognise and target pathogens. |
| Zinc | Oysters, other seafood, meat, chicken, dried beans, nuts. |
Helps keep skin and mucous membranes healthy. |
| Selenium | Nuts (especially Brazil nuts), meat, cereals, mushrooms. |
Zinc and selenium are antioxidants that help neutralise oxidative stress. |
You can find recipe ideas for these foods on No Money No Time, https://nomoneynotime.com.au/ our website developed with support from the NIB Foundation
For a quick nutrition check-up, take our Healthy Eating Quiz
Protect your mental heath with these positive, practical tips from the LoginLab, The University of Newcastle
For almost two years now, our community has experienced cycles of isolation, restrictions, hope that there would be an end in sight, followed shortly by disappointment when the COVID Omicron variant took off. It can be tough to feel motivated. Even tougher once you’ve been diagnosed with COVID-19 and are isolating at home.
Our mental health is equally as important as our physical health and there are things we can do to take care of ourselves and others. For that reason, a holistic approach to caring for both mind and body is important.
If you can relate to feeling overwhelmed and anxious (we certainly can at times), we have some practical suggestions that have come out of our research at the Loginlab, University of Newcastle, and HMRI.
Depending on how sick you’re feeling, you can either dial these up or down to suit your mood.
Plan what you can.
It’s likely that all your routines will have gone off-kilter. That lack of control over our external environment takes a toll on your mental health.
To regain some feeling of control and self-efficacy (shown to be important for long-term emotional wellness), consider making a list of the things you can plan. This might include meal planning or asking your support people to deliver vitamins and flu-relief medication to your door. If you’re feeling up to it, you could even consider doing a gentle online yoga class every second morning (we say this with some authority) or taking up a light hobby that you’ve always wanted to try. Simple, easy routines can have a calming, stabilising effect during these times.
Keep connected.
When you’re feeling crook, it’s usual for people to crawl deep into their beds and not surface for hours, even days. And that’s entirely ok! However, if you find you have an hour or two when you’re not feeling so ‘hermity’ it can be good to reach out to the people you know care about you. It doesn’t need to be an hour long zoom (again, said with some experience of how draining they can be…). But even a quick message, text, or online chat will help you feel like you’re still connected to the broader community. Know who you can message if you feel down.
Keep informed, but not to the point of exhaustion.
Some of our team members choose to have periods not reading about COVID-19 on social media. We found that helpful in re-calibrating how we viewed the world. Consider balancing out the dark news stories with something that makes you laugh, smile or escape. Netflix is there for a purpose!
Take advantage of online clinical supports, if needed
There is still some stigma in admitting we are ‘not okay’ emotionally or psychologically. Thankfully, this is changing. Online programs and chat rooms offer privacy and anonymity and are perfectly placed to use if you are in isolation.
“The good news is that most people who develop COVID-19 will only have mild symptoms and go on make a complete recovery.”
If you have tested positive for COVID-19, the most common symptoms you may experience will be fever, sore throat, headache, coughing, generalised aches and pains, chest pains, breathlessness, loss of taste and smell, diarrhoea, and vomiting.
Professor Wark says that most people will be able to manage COVID-19 safely at home by following these simple wellbeing steps.
Good luck and remember that in medicine the best treatment is always prevention so get the jab, wear and mask and keeping washing those hands!