Our researchers are working to better understand how our immune system interacts with pathogens and the environment, and what impact this has on our overall health.
Our researchers are working to better understand how our immune system interacts with pathogens and the environment, and what impact this has on our overall health.
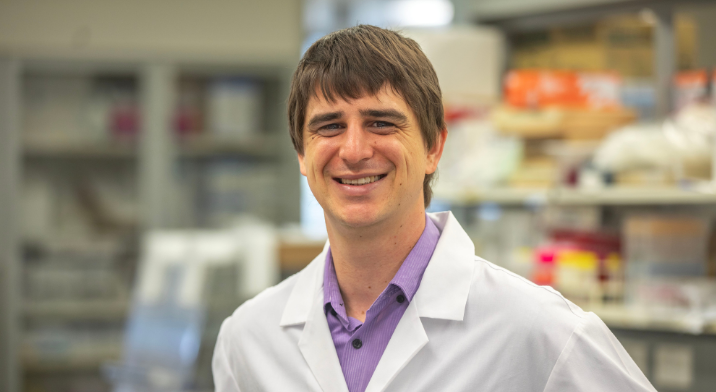
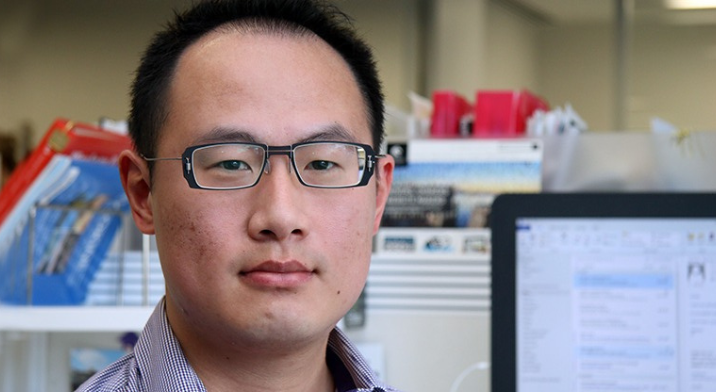
The HMRI Immune Health Research Program brings together scientists, researchers, and clinicians in a collaborative effort to develop innovative solutions for health challenges related to the immune system.
Immune system-related diseases represent a significant health challenge in our community, impacting millions of people around the world.
These conditions include rare, severe genetic immune deficiencies and common, chronic disorders such as multiple sclerosis, gastrointestinal disorders such as Crohn’s disease, allergies, and respiratory diseases including asthma.
1 IN 10
AUSTRALIANS HAVE ASTHMA
IMMUNE CONDITIONS
ARE AMONG THE FASTEST GROWING CHRONIC CONDITIONS WORLDWIDE
90%
OF ABORIGINAL AND TORRES STRAIT ISLANDER CHILDREN ARE AFFECTED BY EAR DISEASE IN MANY COMMUNTIIES ACROSS AUSTRALIA
Despite their prevalence, treatment options for immune conditions are extremely limited. There are even fewer cures.
The frequency of these conditions is rapidly rising, highlighting an urgent need for more effective solutions and personalised care.
Transforming solutions for better immune health
HMRI’s Immune Health researchers are working to transform how we research and treat the immune system.
Our goal is to accelerate discoveries into the underlying features and markers of immune health, to identify disease causes early and target appropriate treatment.
Our program’s research takes a whole-of-system approach, looking at the immune system as a whole rather than focusing on single disease types. We believe this unique approach has the potential to deliver innovative health solutions and transform the immune health of our communities.
Our researchers work across eight key areas:

Aboriginal and Torres Strait Islander ear health
Ear disease in Australian Indigenous populations is far too common and has huge flow-on impacts on other areas of health and wellbeing.
We’re identifying better treatments and preventative approaches for a range ear diseases that disproportionately affect Aboriginal and Torres Strait Islander peoples. The journey of solving ear and lung health issues in Indigenous Australians must be community-led and translated into models of care that have a holistic approach.

Airway diseases and vaccines
Chronic diseases of the airways are extremely common in Australia. Our research is investigating the role of infections and inflammation in the development of asthma and other respiratory problems, including during pregnancy, in cystic fibrosis patients and even in the gut.
We’re exploring the cellular and molecular processes that are associated with the development and progression of respiratory diseases, such as asthma, COPD and more.
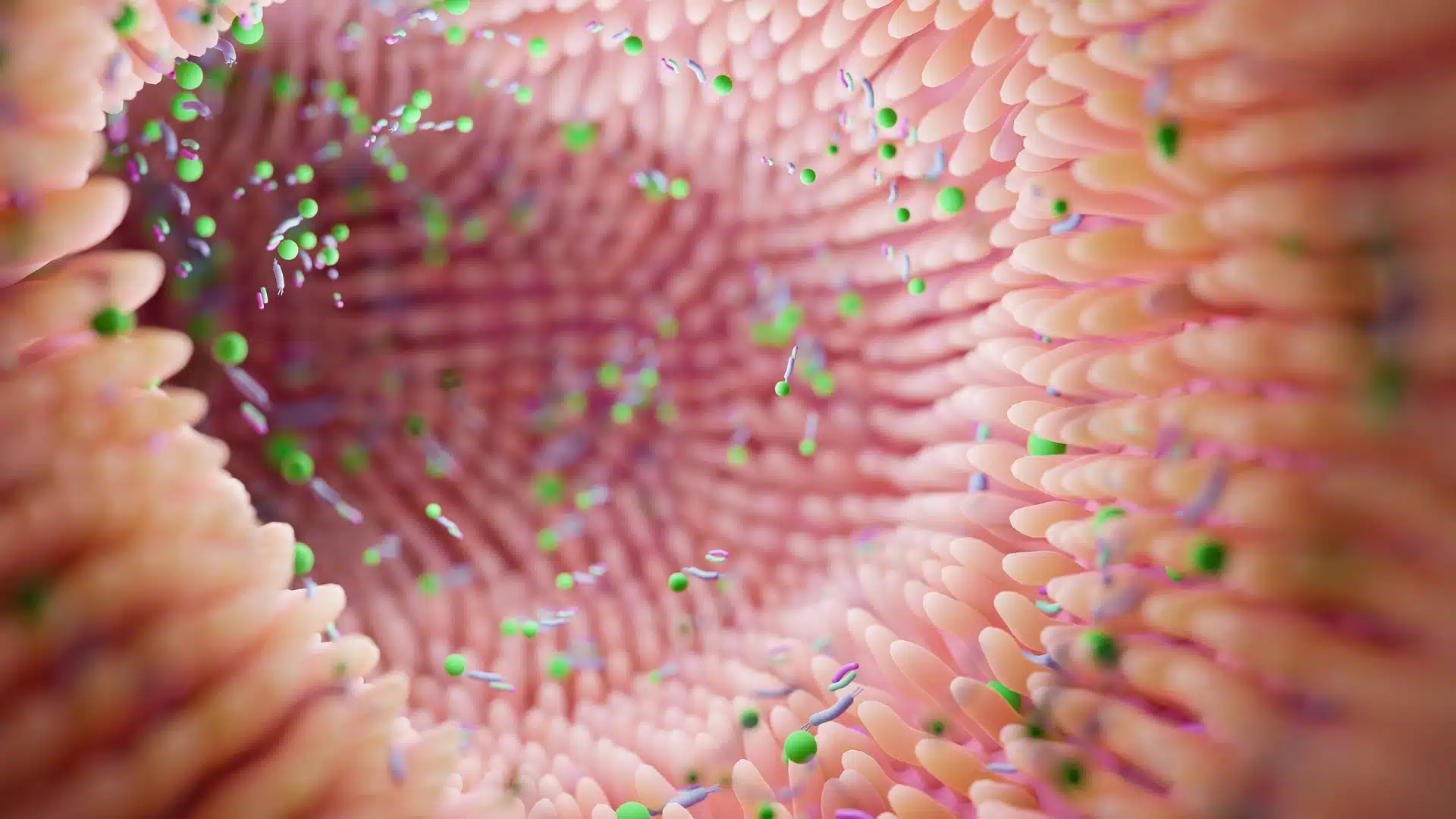
Gut and microbiomes
Gastrointestinal disorders are among the most common health conditions worldwide, but there are few conditions with adequate treatment. And even fewer cures.
Our research is driving solutions for chronic inflammatory diseases such as the inflammatory bowel diseases (IBD), Crohn’s disease and ulcerative colitis – but may also play a role in the development of gastrointestinal cancers. Our team is recognised as a global research leader in this area.
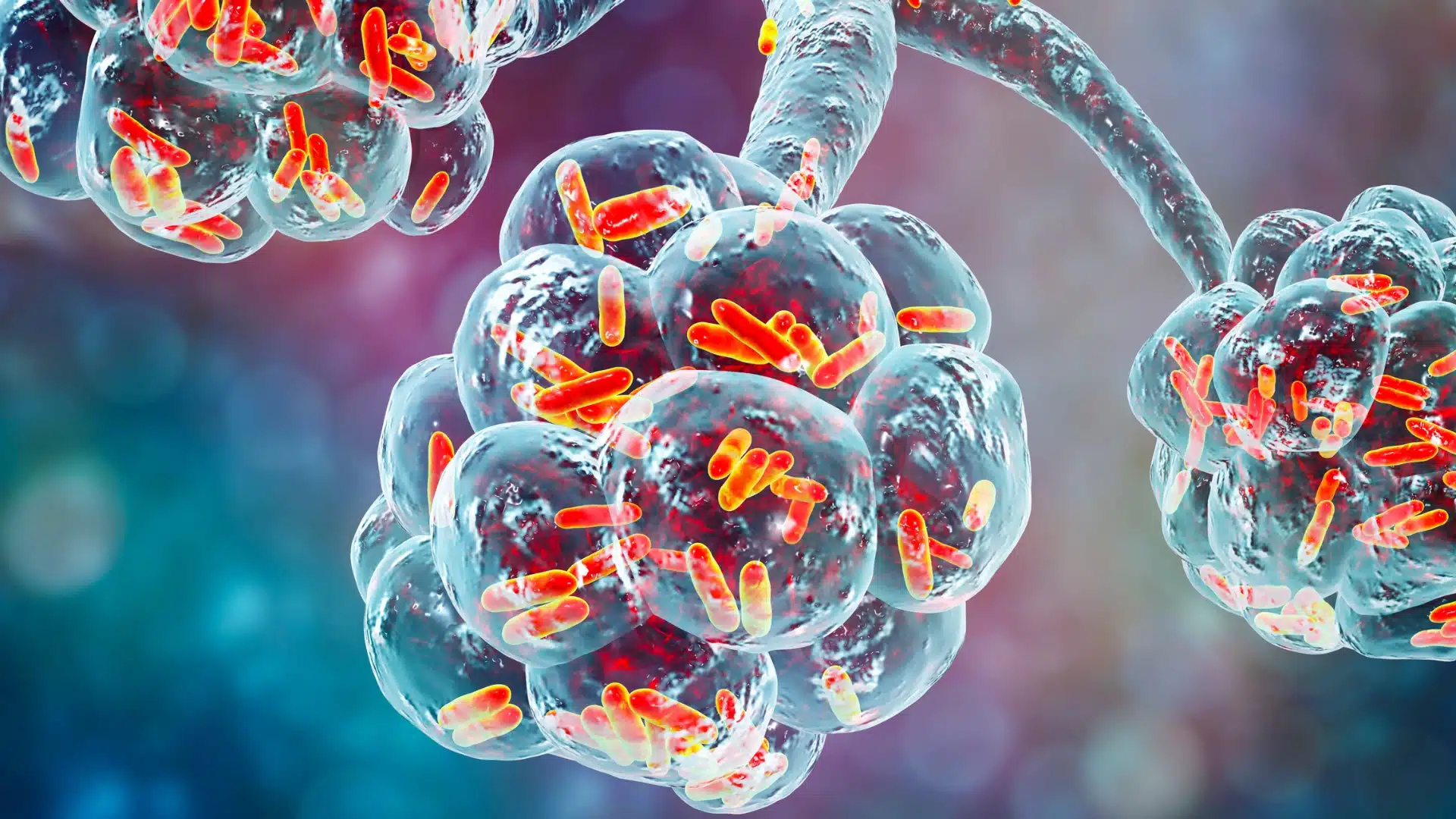
Host, habitat and infection
We’re investigating infections, antimicrobial resistance that affect human health. Our research explores innovative solutions using synthetic biology.
By understanding how pathogens evolve within their environments and leveraging engineered microbes, we aim to develop effective strategies to combat resistant infections and improve patient outcomes.

Neuroimmunology
Our neuroimmunology researchers are examining the link between dysregulations of the immune system and the corresponding impact on neurological disorders (such as multiple sclerosis and dementia, as well as psychiatric diseases including schizophrenia).
Our research is helping better predict and diagnose immune diseases and deliver new treatments that enable optimal immune function in our communities

Nutrition and metabolism
We’re conducting innovative research to understand how nutrition, metabolism, and lifestyle factors—such as obesity, dietary nutrients, gut microbiome, sex hormones, and exercise—affect inflammation, metabolism, and immune function.
Our research aims to shed light on their impact on respiratory virus infections and chronic respiratory diseases.

Stem cells and organoids
Our researcher are using mucosal organoids derived from the lung and gastrointestinal tract to drive drug discovery for conditions like inflammatory bowel diseases, cystic fibrosis, and lung cancer.
We aim to develop personalised organoid assays that enhance precision medicine, currently being validated in a national clinical trial for cystic fibrosis.

Transplant
Organ transplantation is crucial for patients with end-stage organ failure, yet long-term challenges remain, such as chronic rejection and side effects from immunosuppressant medications.
Our research team is developing advanced surgical techniques and medical devices to improve outcomes. reduce injury. We’re also using cutting-edge technologies to discover biomarkers for early rejection detection and explore personalised treatment opportunities.